Explore more on private prisons and reform →
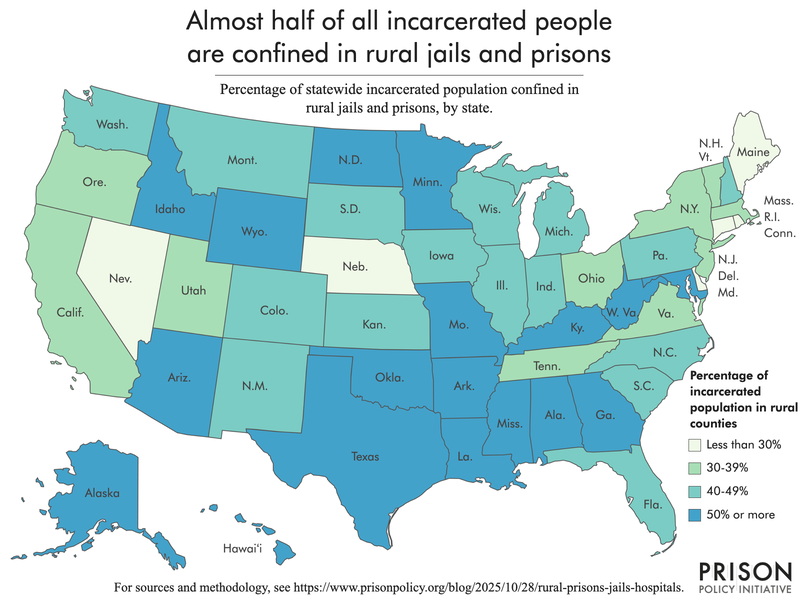
In the United States, nearly half of all incarcerated individuals are housed in rural jails and prisons, often isolated in communities with limited infrastructure and few healthcare options. For these populations, access to medical care is already a daily struggle. Now, proposed federal legislation threatens to make that struggle far more severe.
The Trump administration’s “One Big Beautiful Bill” Act, touted as a sweeping approach to fiscal policy and regulatory reform, could inadvertently accelerate the closure of rural hospitals. While the legislation is framed as a cost-cutting and consolidation measure, the human impact is severe: rural communities, already facing fragile healthcare systems, could see hospitals shuttered, forcing residents—and incarcerated populations—into increasingly difficult circumstances for medical care.
The Rural Healthcare Crisis and Its Consequences
Rural hospitals in America have long been under pressure. Declining populations, lower tax bases, and staffing shortages make small hospitals vulnerable to financial instability. The closure of these facilities has ripple effects far beyond the immediate community:
- Elevated healthcare costs: Remaining hospitals may raise prices to compensate for lost revenue, creating affordability barriers for both residents and inmates.
- Longer travel times for emergency care: Rural populations, already distant from urban centers, may face hours-long travel to reach critical care, dramatically increasing the risk of complications or death in emergencies.
- Limited access to specialized care: Rural hospitals often provide the first—and sometimes only—access to essential services such as prenatal care, mental health treatment, and chronic disease management. With closures, even routine care becomes inaccessible.
For incarcerated individuals, these risks are magnified. Prisons and jails often contract with local hospitals for emergency and specialized care. If these hospitals close, incarcerated people may face delays in treatment or be forced to travel even greater distances under guarded transport, increasing both costs and safety concerns.
Private Prisons and Rural Healthcare Dependency
Many rural jails and prisons are operated or managed in partnership with private corporations. These facilities rely heavily on nearby hospitals to meet legal and ethical obligations for inmate healthcare. When local hospitals shut down:
- Private facilities face higher operational costs: Transporting inmates to distant hospitals requires more staff, fuel, and time, inflating budgets that are often already constrained.
- Healthcare quality may decline: Limited access to timely medical interventions can exacerbate chronic conditions, worsen injuries, or delay treatment for acute illnesses.
- Community and inmate health are intertwined: Rural hospitals serve both local populations and incarcerated individuals. Closing these hospitals risks undermining the health of the broader community and the facilities’ ability to meet mandated care standards.
These challenges highlight a troubling paradox: legislation intended to streamline budgets and reduce costs could inadvertently place both rural residents and incarcerated populations at greater financial, medical, and social risk.
The Scope of the Problem
According to recent data, approximately 50% of the U.S. prison population resides in rural areas. Many of these individuals are housed in private facilities that have limited on-site medical services, relying instead on local hospitals for treatment. When those hospitals close, the logistical and financial burden shifts to the prison operators, staff, and ultimately, the taxpayers.
Moreover, rural communities tend to have higher rates of chronic illness, older populations, and fewer healthcare providers per capita than urban areas. Combining these factors with prison populations creates a healthcare crisis in miniature: an isolated system where access is already tenuous and the stakes are high.
Policy Implications and Urgent Considerations
The potential closure of rural hospitals under the One Big Beautiful Bill Act has broader implications beyond incarcerated populations:
- Public health: Rural communities already face higher mortality rates, and the loss of local hospitals could exacerbate preventable deaths.
- Equity: Incarcerated individuals—already marginalized and disproportionately people of color—would bear a disproportionate share of the consequences of restricted healthcare access.
- Private prison oversight: With private operators relying on hospitals for care, legislation that undermines rural healthcare also indirectly pressures private facilities to cut corners, potentially violating legal obligations to provide adequate medical treatment.
Advocates are urging policymakers to consider these consequences and prioritize healthcare access in rural communities. Solutions may include increased funding for rural hospitals, incentives for physicians to practice in underserved areas, and stricter oversight of private prison healthcare contracts.
The Human Cost of Legislative Inaction
At the heart of this discussion are the human lives affected by policy decisions made far from rural America. For inmates, delayed treatment can mean suffering from untreated chronic conditions, worsening injuries, or even preventable death. For local residents, hospital closures limit access to life-saving care, maternity services, and emergency interventions.
As the debate around the One Big Beautiful Bill Act continues, the fate of rural hospitals—and the incarcerated individuals who rely on them—hangs in the balance. Without deliberate action to safeguard healthcare access, legislation intended to streamline government spending risks creating a far greater crisis in both public and prison health.
A Call for Awareness and Action
This emerging healthcare challenge underscores a critical intersection between private prisons, rural infrastructure, and federal policy. Rural communities and incarcerated populations cannot afford to be collateral damage in the pursuit of fiscal reform.
Sustainable Action Now is committed to tracking these developments, reporting on the human and systemic impact of private prison policies, and advocating for solutions that protect vulnerable populations.
For more coverage of private prisons, rural healthcare, and policy developments affecting incarcerated populations, visit Sustainable Action Now’s Private Prisons section.
The future of rural healthcare—and the lives of nearly half of all incarcerated Americans—depends on timely intervention, informed policymaking, and an unwavering commitment to equitable access for all.